Cephalexin is still one of the most widely used antibiotics for treating a variety of bacterial skin infections, from uncomplicated to life-threatening conditions. In this article, you’ll learn more about it, including how long it takes for it to work.
How long does it take for cephalexin to work on skin infection? Cephalexin takes about 7 to 14 days to work on skin infection. The time it takes for this antibiotic to work usually depends on the type of skin infection and how severe it is.
Keflex is a brand name for cephalexin. It’s generally taken by mouth at 250 mg every 6 hours, or in some cases, 500 mg every 12 hours. More severe infections will require higher doses of oral Keflex at 4 gm daily in 2 to 4 equally divided doses. This antibiotic should be taken for 7 to 14 days.
Cephalexin is available in liquid and tablet forms. Whatever form your doctor prescribes, it’s essential to educate yourself about your medication to avoid misuse or overuse.
Read on to learn more about cephalexin and how long it takes for cephalexin to work on skin infection.
How Long Does It Take for Cephalexin to Work on Skin Infection?
Cephalexin is a first-generation cephalosporin, which is mainly used to treat uncomplicated skin and soft tissue infections caused by gram-positive bacteria. It works in the same way as penicillins by killing invading bacteria (bactericidal).
Cephalexin works by penetrating the cell wall of bacteria. It then binds and prevents the activity of certain enzymes (bacterial-binding proteins) that play a key role in the production of peptidoglycan.
Peptidoglycan, which consists of amino acids and sugars, is an essential component of the outer layer of bacteria. This component provides structural strength to the membrane or outer layer of bacteria.
By interrupting the process of making peptidoglycan, cephalexin weakens the bacterial cell wall and causes it to burst. As you might’ve guessed, taking cephalexin leads to the death of invading bacteria.
So, how long does it take for cephalexin to work on skin infection?
Many factors affect the effectiveness of cephalexin (or other antibiotics). These factors include:
- The specific family of bacteria that’s responsible for the skin infection
- How bad the infection is
- How long it took for you to seek medical treatment
- How keen you are in following your doctor’s instructions for taking cephalexin
- The status of your immune system
Granting that it’s not a life-threatening case of a skin infection, your symptoms might start to subside within 2 to 3 days after taking cephalexin. By day five or six, you’ll most likely feel much better. There are some instances where cephalexin may only start working after a week.
Your symptoms might start to improve before the recommended duration. However, that doesn’t necessarily mean that you’re already free from infection. The improvement in your condition might be due to a decrease in the number of bacteria causing the infection.
So, whether you feel better within a few days or not, it’s crucial to finish your course of cephalexin (7 to 14 days) to prevent bacteria from reproducing again and becoming resistant to it.
Overall, cephalexin is highly effective in treating skin infections caused by gram-positive bacteria (Staphylococcus and Streptococcus strains). It starts working within 48 to 72 hours after taking it, but it may take longer for others to feel improvements, depending on the severity of the infection and other factors.
The following tips can help ensure that cephalexin will produce its intended results:
- Follow your doctor’s recommendations for taking cephalexin. Aside from finishing the entire course of this antibiotic, it’s also important to pay attention to the dosing. Don’t underdose or overdose. If you missed a dose, ask your doctor for advice.
- As much as possible, take this antibiotic at the same time daily.
- Don’t take cephalexin for other types of infection other than what your doctor has prescribed it for.
- Consult your doctor if you experience worrying adverse effects, such as abdominal pain, persistent diarrhea, rash, and/or bruising (or bleeding) during or after a few weeks of finishing a course of this antibiotic.
- Inform your healthcare provider or pharmacist if you’re taking any herbs or herbal supplements, vitamins, or other medications that might interact with cephalexin.
- Examples of medications that could interact with cephalexin are bacille Calmette-Guerin (BCG) vaccine, typhoid vaccine, oral cholera vaccine, metformin (for type 2 diabetes), probenecid (for controlling high uric acid levels), sodium picosulfate (for constipation), multivitamins and minerals, and warfarin (blood thinner).
- People who are reportedly allergic to penicillin are usually able to tolerate cephalexin. However, there’s a small percentage of people who are allergic to both antibiotics. Symptoms of mild to severe allergic reactions to penicillin include coughing, wheezing, extremely itchy and raised spots (hives), lumps under the skin, and throat tightness.
What Exactly Is Cephalexin?

Cephalexin, also spelled as cefalexin, is a prescription antibiotic that belongs to a class known as cephalosporins. It’s sold on the market under the brand names Keflex and Daxbia as a capsule, tablet, and oral suspension. According to Drugs.com, around 10 percent of people who have penicillin allergy will also have cephalexin allergy.
This antibiotic has a high efficacy rate of 90 percent (or higher). One great thing about this drug is that it doesn’t rapidly degrade in stomach acid. For this reason, more of the drug is available for absorption to achieve its intended effects.
As an antibiotic, cephalexin is used for treating a wide array of infections that involve the skin, bones, ears, respiratory tract, and genitourinary system (refers to the reproductive and urinary organs). When it comes to skin infections, it’s mainly effective against gram-positive Staphylococcus and Streptococcus bacteria.
What Are Gram-Positive Bacteria?

Gram staining is a clinical technique that’s normally used to tell two large groups of bacteria apart according to their cell wall. Gram-positive bacteria are those bacteria that retain the primary stain, which is crystal violet dye. Their cell walls are enveloped with a thick layer of peptidoglycan, making their outer structure strong and plays a key role in their reproduction (binary fission).
Examples of skin infections caused by Staphylococcus and Streptococcus bacteria are:
1. Boils
A boil or furuncle is a common staph infection that affects the oil gland or hair follicle under the arms or around the buttocks or groin. In most cases, it may take 7 to 21 days for boils to heal. Recurrence is possible for certain people because they’re carriers of Staphylococcus aureus or simply staph bacteria.
Bacteria can enter the body and cause an infection through broken skin. It starts as a lump, and then eventually, a pocket of pus collects under the skin. Other possible symptoms of a boil are fever, swelling (of the skin and/or lymph nodes), pain, redness, warm skin, and more boils clustered around the original one.
2. Impetigo
Impetigo is more common in children (aged 2 to 5 years) than in adults. It’s a highly contagious disease that affects the superficial skin. Like in the case of boils, a break in the skin—probably from a cut, rash, insect bite, or scratch—gives bacteria an entryway to your body. Once inside, bacteria rapidly grow and cause an infection.
Fortunately, this condition is rarely life-threatening and eventually clears up on its own or through antibiotic treatment (oral or topical). It doesn’t also cause any visible scars.
3. Cellulitis
Aside from the superficial layers of the skin, cellulitis also affects the tissues under it. Early symptoms may include pain, warmth, and tenderness in the affected area, including inflamed and glossy skin, the formation of an abscess with pus, and fever.
Cellulitis ranges from severity, which is from mild to severe (if left untreated). If you don’t seek early treatment, the infection could spread to your lymph nodes, deep tissues, and bloodstream.
Common risk factors for cellulitis include:
- Being overweight or obese
- Having a weak immune system
- History of cellulitis or other skin diseases
- Having lymphedema (a medical condition that causes excess fluid to collect in your tissues, which leads to edema or swelling)
- Having dry, flaky skin, or cracks in your skin
- Using illicit injectable drugs
4. Staphylococcal Scalded Skin Syndrome
The staphylococcal scalded skin syndrome is a serious and contagious skin infection that causes superficial skin layers to peel and blister. Babies and children younger than 6 years old are the most susceptible to this type of skin infection. It rarely happens in adults unless they have a weak immune system or are suffering from a kidney problem.
It can go away without causing any scarring or severe complications, especially if a child gets early treatment. As part of the early intervention, a doctor may recommend antibiotics, fluid replacement, and good skincare habits.
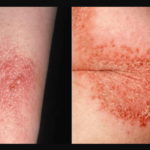
5. Ecthyma
Ecthyma is also known as deep impetigo because it causes erosions of the deeper layer of the skin (dermis). The main symptom of this skin infection is a small blister with a red border, which is similar to that of impetigo. These painful blisters may be filled with fluid or pus.
Treatment depends on the severity of the infection. For early cases, applying topical antibiotics to the infected area may be enough. For severe cases, you may need to receive antibiotics through your vein (intravenous therapy).
6. Erysipelas
Erysipelas is caused by group A Streptococcus bacteria, which usually live on your skin without causing an infection. However, like most opportunistic bacteria, they’re able to penetrate the outer layer of your skin through a cut, scrape, or sore. The common symptom of erysipelas is swelling that’s painful, glossy, and light red skin.
The prognosis in most people with erysipelas is excellent. Antibiotics are usually effective for this skin infection without causing any long-term complications. If there are complications, they’re usually not life-threatening. Sometimes, the infection just goes away on its own without treatment.
7. Blistering Distal Dactylitis (BDD)
Blistering distal dactylitis is characterized by fluid-filled lesions around the posterior fat pad of the fingers. Most cases of BDD are caused by group A beta-hemolytic Streptococci, but in some instances, Staphylococcus aureus (or staph bacteria) could be the culprit. The best way to treat BDD is to incise and drain the lesion and then followed by a course of oral antibiotics and warm compresses.
8. Tropical Ulcers
Tropical ulcers are also known as jungle rot. It’s called a tropical ulcer because it’s a common skin infection in places with a hot and humid climate. The necrotic and painful ulcers usually occur on the lower extremities (ankles, feet, or legs) of children, teenagers, and young adults.
Since it’s a bacterial skin infection, the standard treatment is antibiotic therapy. However, if the ulcers are deep and large, a doctor might perform debridement to get rid of dead tissues.
The ulcers could also heal spontaneously. However, in some cases, lesions may develop in the muscles, tendons, and even bones.
9. Necrotizing Fasciitis
Necrotizing fasciitis, the flesh-eating disease, is a rare but life-threatening bacterial infection. During the early stage of the disease, it can cause the affected area to become blistered, red, swollen, and severely painful, especially after a surgery or an injury.
It’s important to seek immediate medical attention once you suspect you have this flesh-eating disease. Possible treatments for necrotizing fasciitis may include antibiotic therapy (administered into the vein), blood pressure medications, hyperbaric oxygen therapy, surgery, and blood transfusion, just to name a few.
10. Perianal Streptococcal Dermatitis
Perianal streptococcal dermatitis (PSD) is a contagious condition that affects the skin around the anus and private parts in children. It’s caused by group A hemolytic Streptococci, which are the same bacteria that cause strep throat. Common symptoms of PSD are rectal pain, itching, and a moist and dark red rash around the anus. Some children may also experience blood in their stools.
Children with this skin disease usually have a good prognosis. With appropriate antibiotic use, PSD resolves within 1 to 3 weeks. However, it could come back if a child doesn’t learn good hygiene or doesn’t get rid of certain habitual behavior.
Conclusion – How Long Does It Take for Cephalexin to Work on Skin Infection?
So to recap our initial question, how long does it take for cephalexin to work on skin infection? If you take cephalexin every day, it should help reduce or get rid of your skin infection in about 1 to 2 weeks. The type of skin infection, including its severity, will determine how long it takes for it to clear up.
The brand name for cephalexin is Keflex. It is recommended to take 250 mg every 6 hours or, in some cases, 500 mg every 12 hours. Very severe infections may require up to 4 gm of cephalexin daily.
Cephalexin penetrates the cell wall of bacteria, and then it binds and prevents the activity of certain enzymes. See a doctor if your skin infection doesn’t clear up even after taking the recommended cephalexin dosage.


![Neutral Skin Tone Defined [and Best Colors for Neutral Skin] neutral skin tone](https://skincaregeeks.com/wp-content/uploads/2021/05/neutral-skin-tone-150x150.png)